MedPac just did their annual report on Medicare Advantage and they were extremely wrong on several key points.
The MedPac staff has a long tradition of being critical of Medicare Advantage, and they also, unfortunately, have a long tradition of being inaccurate, misleading, and persistently and consistently negative on some key points for no explicable or easily understood reason.
They achieved a new low this year by spending more than 20 pages of the report warning us all in detail about the upcoming cash flow distortions and coding abuses that they say are coming from a risk adjustment model and system that actually no longer exists in 2022 as a functioning system for our Medicare program — and they are also continued their distortion about Medicare overpayment of the plans by running an artificial cost number that functions only to deceive and not to inform and by using what is essentially a fake news number several times in the report.
CMS has now officially cancelled and retired the CMS Hierarchical Conditions Categories Risk Adjustment Model that has been used for almost two decades to calculate risk for plans. It is dead and completely gone for 2022 — and MedPac explained bitterly for more than 20 pages why it was a damaging approach and they somehow did not mention that it was now gone.
CMS has some very good thinking people who brilliantly took that whole set of coding linked issues off the table by making the system that was being potentially abused simply disappear.
MedPac wrote more than 20 pages in this year’s official report about Medicare Advantage complaining about that exact process and system and they didn’t mention that it was gone or explain why it was important to not have that data flow create the risk level information that we will now be using to get diagnostic information into the system.
The new approach for determining patient risk levels is fraud proof. There is no way to put wrong data into the information flow that they are now going to use to see and determine which patients are diabetic and which have heart disease or who has drug abuse issues for the risk discernment processes.
MedPac also had a major content deficit in their report and managed to leave the most important aspects of the work being done now by the plans to help offset some of the damage done to too many Americans who have been damaged by social determinants of health issues for far too long in their lives. MedPac also completely failed to report and discuss the important reality of the fact that we have now reached the point where two of three of our lowest income Medicare beneficiaries are all voluntarily in the Medicare Advantage plans.
They also left out of their report the fact that a significant number of union trust funds and a significant number of employer retirement programs that had made significant promises of retirement health care benefits to their retirees over the past decades are actually having those commitments kept, met, and even enhanced with the relatively new employer sponsored Medicare Advantage plans that work directly with employer settings.
Five million people who might have had their retirement health care programs bankrupt, underfunded, or at serious risk have found a very strong safety net in the Medicare Advantage program — and MedPac does not think that development was important to understand and probably celebrate.
Anyone looking forward at the future politics and funding of the Medicare Advantage program will find both that overwhelming support for Medicare Advantage from our lowest income people and from our most well-connected employer retirement funds to be good and important to understand.
MedPac missed every bit of that agenda and set of accomplishments in this year’s report.
They also left Covid out of the report as a care-related issue and clear difference between the two programs.
They failed completely to explain the huge differences in the care reality, the personal comfort levels, and the direct care availability for Medicare beneficiaries was significantly better on all of the Covid-related issues for the people who were enrolled and given care and treatment in the plans versus the people who were abandoned, isolated, and completely unsupported by the total non-response from fee-for-service Medicare.
MedPac should have used this report to explain what we have learned in that process — but they did not have any portion of the report that related to the impact of either program on actual people.
Leaving the impact of the program on people completely out of the report is not a new trajectory for that MedPac report. They do not see the impact of either program on actual people to be part of their role in advising Congress about Medicare issues.
In fact, they actually tend to complain every year that the vision benefits, hearing benefits, and dental benefits that are made available to everyone and that are appreciated most deeply by our lower income people and that happen only through the plans should not exist as benefits because the MedPac team usually says with a negative perspective that people’s expectations go up if they have eyeglasses and dental work and if they are able to hear and MedPac explicitly does not want to raise expectations of anyone on Medicare.
MedPac is actually consistently, explicitly and directly opposed to people having higher expectations and to better benefits for Medicare in those areas. They believe — incorrectly — that those benefits increase the overall cost of Medicare rather than actually use the Medicare cash flow more consistently and more effectively.
They don’t understand and they don’t believe that the Medicare Advantage plans fund those additional benefits by making much better use of the Medicare dollar. That isn’t additional Medicare money. It results from the plans having costs that are below the average costs for fee-for-service Medicare in each area and it is possible for the plans to do because fee-for-service Medicare buys care badly and delivers care poorly far too often with their much less competent use of the same dollar.
It actually costs less to buy care with Medicare Advantage. The plans have a process where they bid on what their monthly payment will be each year and the average bid is currently less than 85 percent of the average cost of paying for fee-for-service Medicare in each county.
They collect fewer Medicare dollars and they use them far better than those same dollars are used in the traditional payment approach that buys everything by the piece and literally does nothing in any intelligent way to get better value and higher leverage for the money they spend.
We know Medicare Advantage costs less because the bidding process is extremely transparent and open and it openly spends less to get more in plain sight.
The bids are actual bids and they result in actual payments. The MedPac sophists who argue as sophists and as politicized theorists that the money that seems to be spent isn’t the actual cost because we need to re value the dollars with a 9 percent judgement call to see what we are really spending because they are sure that a 9 percent inflation factor needs to be in the calculation even if it isn’t in the cash flow.
It’s a little like the old Marx movie that has MedPac saying: Who are you going to believe, me or your own eyes?
Believe your own eyes.
The bids in about a quarter of the counties fall below 80 percent of the average fee-for-service cost for each county — and stay there each year. When we look at how much we pay for each member, the actual dollars per member that is spent follow the bids — and the actual dollars go down compared to fee-for-service averages in almost all of those areas.
We don’t need to look at projections or estimates or theories on the cost of Medicare Advantage to figure out whether we are paying more or less. We can look at how much we actually pay and add up the dollars.
When plans bid 5 percent less and are paid 5 percent less than we can think of their costs as being 5 percent less.
MedPac does a report every year that contends that the actual amount we pay isn’t the important number for us to understand and we need to do some other calculations to see what the relative numbers actually are.
One report they do every year that distorts the relative cost of Medicare Advantage compared to fee-for-service Medicare looks at the actual care given to Medicare Advantage members and then prices that care using the Medicare fee schedule.
They look at Medicare Advantage enrollees and they look at their exact pattern of care and then they price that care using the Medicare fee-for-service fee schedule. They then compare that number with the capitation paid to the plans for those people and show that the numbers are consistently very different every year.
Using that model — and not adjusting it for the actual change in patterns of care — it generally looks like it costs about 4 percent more to pay the capitation than it costs to buy care for those people by the piece.
They love doing that report. It’s in this year’s annual report three times. The reality is that the care is far better for the Medicare Advantage plans and that’s the pattern of better care that gets priced by that process. The relevant numbers are all consistent and obvious.
Medicare Advantage has about 35 percent fewer emergency room days. That’s true every year. Medicare Advantage has programs to reduce the crisis level congestive heart failure events and that tends to result in 40 percent fewer hospital days for those patients. Medicare Advantage plans have many more e visits fee-for-service Medicare does not pay for e visits.
When MedPac does that cost comparison every year, they don’t have those emergency room visits in their care pattern, and that means that it looks like fee-for-service Medicare would have spent less on those exact patients.
They actually call that the overpayment report — and it typically shows that the Medicare would have spent about 4 percent less on those patients if the only care-related cash flow in their lives was the benefits that were included in the limited and standard traditional Medicare fee schedule and purchased by the piece for those exact patients.
It’s important for them to use the exact patients for that calculation, because when you use any other measurement, Medicare Advantage costs less. The capitation is lower than the average cost of care in all of those counties. That is extremely visible as an expense.
The plans each look at the average cost of fee-for-service Medicare in each county, and they get a chance to bid each year against those average costs and they always bid much less.
In the highest cost counties for fee-for-service, even this year’s MedPac report shows many plans bidding 40 percent less.
The actual capitation that is paid to the plans each month is legitimately based on the actual average cost of care for fee-for-service Medicare in every county. That is a good, useful and important number and when we are looking at how much we are spending on each program, that average number is a very legitimate benchmark for figuring out if we are getting a good deal financially for the program.
They actually label that the benchmark process and it creates the benchmark prices that are used for enrollees in each county.
The capitation money the plans are paid each month is used by the plans to provide care, and the plans can be very flexible in how they use that money. The plans have to provide the basic set of Medicare benefits and they also need to do some defined and expected levels of quality and service reporting for that money, but they can use it in very flexible ways to provide care to their members.
They can use that money to provide additional levels of care and they can also use any and all legal caregivers available to them to serve their members in the process. A Medicare Advantage plan might send a nurse into a home to help with a diabetic patient or to help avert a potential congestive heart failure crisis, and they can pay that nurse to provide that care from the capitation paid to the plans. Fee-for-service Medicare does not pay for those nurses or for those sites of care — and fee-for-service Medicare would even accuse, charge and possibly indict that nurse for Medicare billing fraud if the nurse performed those same services and then sent a bill to Medicare for their time and efforts.
So Medicare Advantage patients tend to have both better care and more flexible care at several levels compared to fee-for-service Medicare patients. The plans also have quality reporting and expectations that does not exist at any level today in fee-for-service Medicare and that makes the MedPac comment in the report about the quality differences being completely non-discernable are discernably wrong.
We know from the current five-star reporting system that Medicare Advantage plans increased the percentage of cardio vascular patients who were receiving and using their statins from 80 percent to 83 percent even under Covid situations last year — and we know that the diabetics in Medicare Advantage plans lost ground on having their blood sugar controlled and the Medicare Advantage plans, on average, had that number with blood sugar controlled drop from 80 percent to 76 percent of the diabetic patients under the Covid year.
So, even though the plans did far better than fee-for-service Medicare in responding to the immediate care needs of their Covid patients, we know that they lost some ground on some levels of care during that time.
Fee-for-service Medicare, by contrast, actually does not have one single quality measure.
None.
Fee-for-service Medicare simply does not do any quality improvement programs. They also don’t set any quality goals, and fee-for-service Medicare does not support or pay for team care or for medical information pooling and linkages for their patients for use in care quality activities for their caregivers.
The MedPac staff wrote again in their report about the status of Medicare Advantage that they could not comment on the quality of care in fee-for-service Medicare compared to Medicare Advantage because they have no data for those fee-based patients, which means that it is impossible and wrong for MedPac to comment on the comparative quality of care. They believe and they say that clear deficit in quality data that exists for fee-for-service care sites and those caregivers should not cause anyone to conclude anything about the relative quality of the two programs, or should be a reflection in any way on any part of the fee-for-service Medicare, because that would be “unfair to fee-for-service Medicare” to point that data issue out in any public way.
That avoidance of the quality issue is just wrong.
We clearly do have significant levels of quality data about the Medicare Advantage plans because we have extensive levels of quality program and recognitions that exist in Medicare Advantage. Those programs get better every year — and MedPac should be reporting and even celebrating each year how many additional plans are achieving high scores in those areas as part of their report.
MedPac should be describing and celebrating progress that is being made in that five-star space and the members of the Commission don’t seem to know that information exists.
In fact, they sink lower than that pure denial in their report this year. They actually say in this year’s report that they have deep concerns about the quality of care for Medicare Advantage and they say clearly that they have no useful data to use for thinking about how Medicare Advantage is doing relative to quality issues.
Saying that there is no quality data about the plans is another MedPac falsehood (MPF) and, as they so often are, that particular falsehood is disproved quickly and easily by their own documents. In the final section of this year’s report where they were asked by Congress to do a report on the quality of care in the Special Needs Plans. The MedPac writers achieve that explicit goal in large part by using the easily available HEDIS quality data for those patients and for the other patients in the plans and by comparing both sets of numbers to relevant populations.
So this year’s report has that set of NCQA quality data for the Medicare Advantage plans included in it. MedPac is using it now even though they say no data exists and that means that’s another falsehood to say it doesn’t exist.
We know what the quality data of the five-star program is and we know what the HEDIS Scores are for the Medicare Advantage plans, and we also know how much Meicare Advantage costs us in every county because the bids give us that information.
We know that the plans bid below the average county fee-for-service Medicare costs are in every county and we know what the total costs are by person for each county.
We need to know what the real costs are and we need to look at how we get the very best use of the Medicare dollar. MedPac should make it a priority to figure out how to get the best use of the Medicare dollar using both bids, capitation, and various kinds of ACO-related payment processes. ACOs all create better care than traditional fee-for-service Medicare, and the people who are critical of ACOs for not saving enough money should rethink their priorities and they should be happy with any use of the Medicare dollar that gives more for the member and patient
If an ACO that has team care and patient centered data flows just breaks even on costs relative to fee-for-service Medicare, that should be celebrated and supported as being a much better use of the Medicare dollar.
We should make patients our top priority. ACOs make patients their priority. Medicare Advantage Plans clearly set up benefits and care practices around the patient’s the top priority. Only fee-for-service Medicare completely lets the patient down by being rigid on benefits, rigid on service, and making costs a higher priority than people’s lives and doing that badly and inefficiently.
We should be working through MedPac each year to see which approach to buying care actually gives us the very best use of our Medicare dollar.
The annual bidding process for the plans is important and it is not very well known to most policy people or to the news media in our country today. It directly anchors costs for every county for every Medicare Advantage member.
The plans each bid an amount in each county that will determine what they get paid in each county for each enrollee. They receive their capitation amount every month, meet the administrative and care delivery requirements that outlined in their Medicare Advantage contracts, provide all levels of needed care, and then they either make money or lose money on their bid.
That bid is a very powerful, important and relevant tool, because the capitation, itself, is the total amount that Medicare will ever have to pay for each Medicare Advantage patient. That cost control impact is an important point to understand. That bid and the capitation it creates actually caps costs and it defines costs for that patient.
Unlike fee-for-service Medicare — where the caregivers can and often do make much more money when their care fails because failures of their care in fee-for-service health care often increase the number of fees that are paid for a patient — the capitation to a plan is the full cost to Medicare for that patient and it can’t be increased in any way.
A congestive heart failure patient goes through pain, dislocation, and sometimes even fear of dying or fear of being permanently damaged when they have a congestive heart failure crisis — and the plans actually can save both money and save lives by not having those crisis happen.
Those very same heart failure crisis are often very profitable for fee-for-service Medicare care sites because they can and do generate from $20,000 to $40,000 in additional revenue for the care sites when they happen to occur for patients.
So, Medicare Advantage plans all build congestive heart failure crisis prevention protocols and fee-for-service Medicare does not even support or pay for the steps needed to put those processes in place.
So when the MedPac staff writes, as they actually do each and every year, that there is no fee-for-service quality data available and therefore they can’t comment on the relative or relevant quality issues for Medicare Advantage plans because those comments would be inappropriately unfair to the fee-for-service Medicare program, that is another inexplicable part of the MedPac thinking and to their approach to reporting on Medicare Advantage and it’s an area we should change before they write another annual Medicare Advantage report.
They also inexplicably, unfortunately, and very completely ignore actual people in their MedPac staff annual report on Medicare Advantage.
They have no part of their annual report on Medicare Advantage that deals with the issues and the impacts of any of the actions or issues or processes on actual people and their lives. They have managed to write an entirely people free report as their annual advice to Congress about Medicare Advantage program, and their advice to Congress has a major hole in it and an obvious deficit because they have chosen to keep people and their lives out of their report.
That does not seem possible, but it is clearly true and it is clearly intentional because the people gaps are so obvious and visible.
Covid has just done damage to a lot of people in our country. Covid has been a major issue for people’s lives and for people’s care over the past couple of years. The MedPac report completely skips the topic of Covid impact on people except to speculate about whether Covid might have affected costs for either program in some way.
In the real world of people, there often were huge and obvious differences between the Covid responses of the Medicare Advantage plans and Covid responses of fee-for-service Medicare. A people-oriented annual report from MedPac on Medicare Advantage would have looked at those differences and pointed them out as very different uses of the Medicare dollar that happened down each of those payment pathways.
Every Medicare Advantage patient had a complete care-related contact system and support processes that were consistently in place for Medicare Advantage patients immediately. Medicare Advantage plans were recognized for being among the very first care sites in the country to have some of the Covid tests in place and they even sent nurses into some homes to help with care very early in the process.
Every single Medicare Advantage member had the security from day one of knowing where to go for their Covid care. They all had care sites immediately because they were all members of plans, and those care sites and care systems in the plans all went through their own learning process to figure out the relevant Covid-related issues of care.
Fee-for-service Medicare had nothing.
Fee-for-service Medicare had no Covid plan or Covid-related approach. Fee-for-service Medicare left many people functionally orphaned and isolated because the fee-for-service enrollees who already had some level of care relationships in place could try to get into those sites but the people with fee-for-service Medicare Coverage who did not have care linkages in place were simply orphaned by Covid. They had to scramble on their own to find Covid care and information with literally no support from fee-for-service Medicare.
MedPac is supposed to be writing a report evaluating Medicare Advantage.
This year’s MedPac report should have led with a report and an update on Covid in those various settings and it should have included an informed discussion of what we learned in the process — and MedPac completely and carefully dodged the issue. It wasn’t even mentioned because MedPac does not mention or include people in their report in any case and it is also much easier to continue to be generically critical of Medicare Advantage if you leave people and their lives out of your analysis, research, thinking, and report.
What they did mention, in several places and in multiple pages of the report, was that they believed that Medicare Advantage capitation is too high and they stated that the capitation is more than Medicare would have spent for those same enrolled people if they had not enrolled in Plans.
They stated a couple of times that when they looked at how much fee-for-service Medicare would have spent paying for care “for those same exact enrollees,” it appeared to them that that number spent to buy each piece of the care that actually happened for those Medicare Advantage members was lower than the actual capitation that was paid to the plans for those exact same enrollees.
They estimated from that particular calculation that it cost about 4 percent more in capitation last year than Medicare would have spent buying those exact sets of Medicare services for those same patients if the people had not been enrolled in the plans.
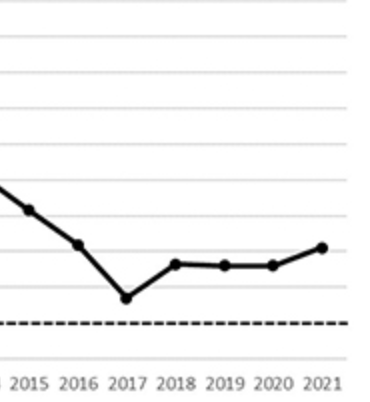
They repeat that perspective and that conclusion several times. It’s also actually almost the only line chart in the entire report. Figure 12.4 has the number. They run the numbers back to 2004 to show that the number has existed as a difference between those calculations every year and that the distance been consistent over time.
That chart and conclusion gets quoted in multiple settings in health care policy circles as being basic context for whether the plans are overpaid and many people in both media settings and academic settings believe that number to be true and cite it in various places.
The problem with that number and with that calculation is that they very carefully price only the exact pieces of care received by those members and some of the most relevant pieces of care do not happen for those exact members because care is actually much better in Medicare Advantage plans. The capitation calculation numbers that create the baseline data and the bidding floor for each county are inclusive average numbers for the fee-for-service Medicare patients in each setting and they are based on and include the higher costs of poorer care that generally is delivered in fee-for-service Medicare.
The differences are easy to see and understand.
Medicare Advantage members have about 35 percent lower use of emergency rooms. They also have significantly lower numbers of congestive heart failure crisis. The fee-for-service care that was the basis for the capitation calculation and baseline number had all of those higher expenses from emergency rooms and congestive heart failure crisis built into them — so that means that the only way that number from figure 12.4 can legitimately be used by MedPac to evaluate the relative costs now would be to add the relevant ghost numbers for those better care patterns back into the amount to show the cost that Medicare would actually have spent for those patients if they had not been enrolled in plans.
The MedPac staff clearly knows that those are fake and deceptive conclusions about the patterns of care and about the relative costs of the programs because they actually say very clearly in this year’s report — toward the end of the report in a discussion on another topic: “Plans steer patients away from an emergency department when an urgent care clinic or physician visit would suffice and is available.”
So even this report as written shows that they know that truth about those care pattern differences.
They very carefully tee up the illusion of a higher payment level for capitation each time by saying: “This is exactly what those exact same Medicare Advantage patients would have cost if their exact levels of care had been purchased by fee-for-service Medicare using the fee-for-service fee schedule.”
That is only legitimate information if they add to that cost number they compute for the current enrollees’ levels of care by putting those emergency room visits back into the cost total.
The average difference in costs of care that should be added back into that calculation to make the conclusion and to make the comparison with current members costs legitimate is actually about 9 percent additional costs — based on other available data.
Without that 9 percent, this is false information and it is fake news.
What is true about the relative cost of care for people who enroll in Medicare Advantage?
That is actually also relatively easy to see and know and it is also already embedded in this same report at several levels.
The bids are key.
The bid process and the numbers that relate to it already show us how much different the costs are for Medicare and for Medicare Advantage. The average area’s costs for fee-for-service Medicare are very legitimate costs and they anchor and tee up the process and the bids then create the actual cost of Medicare Advantage measured in real dollars.
The plans bid each year for every county and those bids both indicate what the cost differences are and what they have created in each county as the total cost each year to Medicare. We don’t need to guess or approximate or estimate the costs of the plans to Medicare because we now pay them in capitation each month. We don’t need to speculate about how much the plans might somehow cost us in total because the bids result in a capitation and because the capitation that is paid creates the actual cost and we know exactly what those capitation payments are.
So what are the bids?
The plans actually bid less than the average cost of care for fee-for-service Medicare in each of those areas.
The plans this year bid an average of 86 percent of the average Medicare fee-for-service costs in the counties.
That means that if nothing else changed, Medicare would spend 86 percent of what it spent last year to provide care in that county for those enrollees.
That initial bid isn’t the final cost. Medicare Advantage has what is probably the best quality assurance program of any government purchased care program in the world. That program includes a five-star process that tracks care and service and actually awards plans from one to five stars for their measured levels of performance, and then pays more money to the plans with more stars.
Those standards set by that program have a huge impact on American health care because so many care sites are involved in Medicare Advantage as their source of payments and patients and because so many care sites have done very intentional and explicit work needed to earn the stars.
Thousands of care sites linked to Medicare Advantage plans have a chance to do better on their payments and their cash flow if they manage the blood sugar levels of their diabetic patients well, and the care teams get better every year in delivering that care and making sure their diabetics have care teams focusing on their care and getting it right.
Diabetes is the number one cause of blindness in the United States. Diabetes is the number one cause of amputations in America and it is also the top priority and most damaging co morbidity for causing death from heart disease. It is a very good thing that we have a five-star program in Medicare Advantage that encourages large numbers of doctors and many care teams in many settings to provide better care for their diabetic patients.
Those Medicare Advantage quality programs sometimes also have an extremely positive spillover community benefit impact on all patients in a care site or a community because the doctors in each setting prefer to practice consistent care and that level of better care rewarded by Medicare Advantage tends to be extended to all of the patients in those sites and settings. Several studies have shown very positive quality improvement spillover impacts exist on high volume Medicare Advantage counties from those programs.
Medicare Advantage pays money for that to happen.
Higher scores on the five-star quality results can and do actually significantly increase payment levels for plans. Plans can earn up to 5 percent more dollars by having more quality stars.
That program has probably had the biggest improvement on care quality for large populations and for a wide range of care teams of any other single program in the world and it has actually changed care at levels we can see and track over time. Again — the evidence on how well that program is doing is hiding in plain sight.
When the program was first started, less than a dozen very high performing plans in the entire country earned five stars and very few plans even had four stars. Plans and care sites across the country have worked hard and very intentionally on those quality processes since that time and today we have reached the point where more than 70 percent of the Medicare Advantage members are now enrolled in four- or five-star plans.
That is a major and visible improvement. CMS appreciates that progress and CMS has done wonderful and increasingly effective work in encouraging and supporting those levels of performance improvement in the care sites — and the teams of people in those various administrative jobs at CMS have been using those approaches to encourage and support better care for a growing number of people.
MedPac, however, doesn’t even seem to know that they exist or what they do. The MedPac commissioners don’t ever talk about those parts of the Medicare Advantage program in their meetings and they don’t seem to have any knowledge that those programs or measurements and culture changes for care sites that have roots in Medicare Advantage even exist.
It’s not damaging the country or the overall program for MedPac to have a high level of ignorance about those issues because the people who actually run Medicare for CMS do understand the tool kit completely and the people in those leadership positions at CMS understand and support the approaches and use them well.
The people who run CMS will probably enhance several pieces of that process at this point for the Special Needs Plans in very high impact ways, and care will improve for that very important population of people as part of that agenda and of that focus by CMS.
MedPac, by contrast, has an almost inexplicable void in that area in their thinking and in their annual report.
What is on the MedPac radar screen and what keeps their attention and what actually takes up several long portions of the annual report this year is the other factor that changes the payment levels to the plans — the risk status of their enrollees.
The capitation levels that are paid to the plans are affected very directly by the health status levels of the actual enrollees.
Risk levels for the members set and change the payment levels for the plans. The very first capitation programs didn’t factor in relative risk status for the members, and it was possible for some care sites to make major profits on capitation just by enrolling healthier than average people and by being paid an average cost level for each area for the people they enrolled.
That initial payment process has evolved very intentionally into having diagnosis-based cost factors that attempt to link the health status of the members and a fair payment level for the plans. The plans identify for the risk filing process the diagnosis levels for the members and their payment levels as plans are directly affected by the risk levels they report for their members.
People have had some concern about whether some parts of that coding process have been done badly, incorrectly or with purely avaricious intent.
There have been significant levels of concern expressed about whether the plans might be able and willing to produce and present inaccurate and distorted information in the process. That alarm was triggered in part by the fact that some of the plans made getting that information into their annual filings a high priority and some were more successful than others in that process.
It is good to have accurate diagnosis information.
We actually should as a nation and a health care macro system want to see an expansion of our data base and our medical records on basic levels of diagnostic information.
As a nation and as a macro care system we should definitely want to have full diagnosis information for each patient. Care can be better when caregivers have the right diagnosis for all of their patients.
CMS just did a brilliant thing and completely eliminated the filing system and process for risk coding and data.
The CMS Hierarchical Conditions Categories Risk Adjustment Model was just killed. CMS just took the system that has created the vast majority of concerns and churn about the issues of coding intensity and shut it down.
It no longer is a factor for any risk scores. CMS will still look at the relative risk levels of patients but will get that information completely from patient encounter filings and direct patient information and not from any plan filings or reports.
An entire industry of organizations working to enhance risk scores just became obsolete and irrelevant.
That was a wonderful thing to do because we can now focus on having the best care and the right payment levels for people where we have no doubt about the diagnosis and levels of care.
That makes 20 pages of this year’s MedPac report completely irrelevant to any parts of the new risk payment processes.
MedPac knew that was happening — and a much better report would have looked at the new issues that are created by that flow of data about diagnosis and risk.
All of the concern about whether nurses gather accurate information about diagnosis in home visits is no longer a coding concern and it is now, very appropriately, a care delivery issue and a care improvement concern.
No caregivers under the old model actually invented diagnosis. That accusation was made in fairly public ways a number of times. It was also fake news. For a very good reason. The medical records are considered almost sacred records by the caregivers in actual care sites, and the likelihood of caregivers putting fake information into that sacred and highly functional and carefully protected work space simply to distort risk codes for health plans is actually very low in the real world.
MedPac said in one critical part of this year’s report that the discernment process on diagnosis only flowed in one direction and MedPac pointed out that the process didn’t provide for the nurses who were doing the health assessments in the homes to change the initial medical record if the nurse discovered in the home that the patient was not actually diabetic.
That particular concern about the one-sided directional flow of the coding process by MedPac does not understand that the likelihood of a nurse in a home changing the medical diagnosis of a patient that had been done by another caregiver is pretty close to zero because nurses aren’t allowed or in any position to change that information in a medical record and we would actually would not want that change in our medical records to be allowed or to happen.
Some people will still be concerned that as long as plans are paid more for having patients with certain diagnosis, the number of patients with those diagnosis might explode. It probably will expand, but there is a very good reason why it won’t explode.
The biological reality is that we humans have a limited number of diagnosis to discern and once they are discerned for each of us, that particular data burst is done and it won't grow much from that point on.
When the new coding process kicked into gear, auditors looked at Medicare Fraud issues and some auditors estimated that basic Medicare billing fraud runs about 6 percent of fee-for-service Medicare and those first auditors also estimated that 6 percent of coding fraud probably also existed for Medicare Advantage.
The billing level fraud will probably continue — because it is so hard to stop — but the 6 percent matching fraud on coding has just ended.
When that report was written, the auditors said that the only sure way of getting rid of any coding fraud would be to build the data flow into the actual encounter system. The people who run CMS clearly read their own audit and then just did exactly that. They should be able to score a zero in that category for this year’s filing — and that is not insignificant progress.
Well done, CMS.
The current MedPac report has not figured that out and the report is still deeply concerned about possible coding fraud. They can probably relax and the fraud issue should look very different for next year’s report.
So the 6 percent coding fraud number and the 9 percent risk inflation number are now both irrelevant and both should be off the table for the next report.
So what are the real costs of Medicare Advantage?
Medicare Advantage costs less.
Medicare Advantage costs a lot less. When the plans did their current bids, they ended up averaging 86 percent of the fee-for-service cost averages. They offer much better benefits, much better care, much better patient support, and they cost members nearly $1600 each in lower direct out-of-pocket costs.
The plans are much more effective users of the Medicare dollar than fee-for-service Medicare, and the plans generate surpluses for the members from that lower capitation level that this MedPac report says average more than $300 a month.
This report acknowledges the record levels of surpluses. Each of those surpluses represents Medicare Advantage costing less than standard Medicare because they come from the capitation and they are absolutely a better use of the Medicare dollar than fee-for-service Medicare gets from spending that same dollar.
Plans have created a record number of surpluses each year and they all come from spending fewer dollars per person than standard Medicare. Fee-for-service Medicare is a very poor purchaser of care — and that fee-for-service Medicare program now has its average member each spending more than $5000 in out of pocket costs each year because it is an inferior way to buy care.
When we look at the lower amount we are spending on capitation in all of those counties, it is easy to see that Medicare Advantage costs less. We can use that money going forward as our pathway to bringing Medicare spending to much better levels as a country.
We don’t need actuarial estimates of relative values of some kind to measure the actual impact of the costs. We can do just like anyone else buying coverage does and measure the difference in actual dollars against the alternative costs of the competing program and we can look at how much the actual dollars go up from year to year for each county in the country.
That’s the number we need to bring under control and we can do it by setting the capitation at the right level to achieve that goal.
The average per capita costs of fee-for-service Medicare are a very legitimate measure of the cost of the program and we know from that data that Medicare Advantage costs less. We need to build on that success.
People who don’t want to accept that reality can do various creative approaches to distort the costs of each program by inventing pseudo risk adjusted surrogate expense levels for the comparative calculations, but Medicare itself actually spends real dollars and not pseudo surrogate dollars and we know from looking at the data outlines in this year’s report that Medicare spends about 10 percent less per member right now on Medicare Advantage than it spends on fee-for-service Medicare in all of those counties.
If you pull the target expansion counties and that program out of the Medicare Advantage payment flow and calculations, the average cost in the other counties ends up significantly less than 90 percent of the actual average cost of care for fee-for-service Medicare in those counties and that is measured in real dollars.
Those numbers are all in this year’s report — hiding in plain sight.
The biggest gap in the MedPac Medicare Advantage report this year is to miss and not report the extremely important and extremely relevant fact that two out of three low-income Americans have now joined Medicare Advantage.
All Medicare Advantage members are not the same. Two out of three of the lowest-income Medicare members are now in the plans.
More than half of the African American members of Medicare are now in the plans. We have now also exceeded to the point of having more than 60 percent of Hispanic Medicare members in the plans.
More than two of three of the lowest-income members from all groups have joined Medicare Advantage plans.
Much better benefits for Medicare Advantage plans make that enrollment by our lowest-income members happen. When the average net worth level of the Hispanic Medicare Advantage member is actually $12,000 — then the fact that the Medicare Advantage plans are language proficient and actually offer vision benefits and hearing benefits and dental benefits is hugely important because it’s functionally the only way that some of those members are ever going to be able to see and to hear.
The MedPac staff who are advising the Commission and the Congress with this report continue their tradition of leaving people entirely out of their report and entirely out of their priorities and they also believe and continue to say that those eyeglasses somehow indirectly distort and somehow increase the overall costs of Medicare because they exist and therefore they must cost Medicare money in some way and they don’t want Medicare to pay for anything that wasn’t in the original set of Medicare expenses.
That is just plain wrong thinking. Coldhearted, callous, sad, short-sighted, and wrong.
The Commission should ask their staff after reading the report this year to change their priorities and to make helping people and improving team care and improving personal care for people a priority for the use of Medicare dollars instead of resenting and literally disparaging those efforts and those approaches that improve lives because those enhancements increase enrollment in the plans and the staff writing those pieces of the report clearly does not want that enrollment to increase.
The most important work done by Medicare Advantage this year again is actually the Special Needs Plans, and the MedPac report team left them also entirely out of their report
We have a lot of people in this country who have been damaged for too many years in too many ways by social determinants of health factors that have created inequities and disparities in both health and care.
A high percentage of those people who have been damaged by social inequities of health are people who are eligible now for both Medicare and Medicaid. The dual eligible people have some of the biggest health care needs in America and the people with those needs deserve our support and our best efforts on their behalf.
Medicare Advantage is helping in a major way right now — and that was not mentioned in the report.
The Medicare Advantage Special Needs Plan people who are eligible for both Medicaid and Medicare need our support more than anyone in the country and it was a particular blessing that we managed to get nearly 4 million people into those plans before Covid hit.
We are blessed to have had that opportunity and we need to make the people who are in both Medicaid and Medicare a priority.
CMS today clearly understands that situation. Very good and caring people at CMS and the Medicare program are working on and with the Special Needs Plans now to make a major difference in the lives of millions of people who very much need that difference to happen.
The MedPac report — continuing its multiyear practices of not placing any priorities on real or actual people or on any part of their functional lives — sadly managed to leave one of the best things we are doing in the country as a government to functionally, directly and individually remediate social determinants of health damaged people completely out of their annual report.
MedPac exists to advise Congress. Most members of Congress care very much about people’s lives. We need whoever provides oversight to the group and that Commission from Congress to ask MedPac to add that priority and those actual impacts on people of Medicare Advantage to next year’s Medicare Advantage report.
The 400 Members of Congress probably would not be happy with a MedPac recommendation that suggests the benefits for the lowest-income people should be reduced because the benefits are attractive to too many people and get too many people to enroll in those plans.
‘Tone deaf’ comes to mind as a level of priorities and a descriptor for this year’s MedPac Medicare Advantage report.
So this year’s report has flaws.
But —
We are at the point in the history of American health care where we could actually be on the cusp of a golden age for care. Our medical science is exploding. Beautiful tools are emerging and are becoming available to us. Our ability to do better diagnosis and to do better care — with better connections between caregivers and between caregivers and the patients they serve — has never been as good as it is now and it is going to get even better going forward from now.
We have up to a third of the people who are dying in hospitals who have had wrong diagnosis along the way to their care. That should not be happening. We need better data, better outcomes, better connections, better diagnosis, and better care, and we need to spend less to get more because the science should make that entirely the path we are ongoing forward from here.
We should be using artificial intelligence to build care agendas and treatments for people and to provide the very best care at the very best sites of care. Some care site programs today are actually providing fully connected in home hospital care that has better outcomes and much lower costs than most traditional in hospital care and that should be available broadly and soon because the people doing that work are beginning to do it to scale.
That is relevant to this report on the MedPac annual report on Medicare Advantage because Medicare Advantage should be a major asset in making that new world happen.
Fee-for-service Medicare has crippled far too many care enhancements, but Medicare Advantage should be a platform for making that better future happen.
MedPac should help by learning now what that continuum of possibilities actually is and MedPac should become expert in their applicability of all of those resources to both Medicare Advantage and Medicare itself.
ACOs should be data enhanced. Plans should insist on and deliver continuously improving care.
The new tools will be entirely transformational. We should use the huge cash flow of Medicare to help make that happen and when we do that well, care will be better and much less expensive for everyone.
So MedPac — please move on and please make a major difference in the future delivery of care because we need continuously improving care and that will only happen if we do some smart things to make it happen.
And stop using cost numbers about Medicare Advantage and process warnings about possible cost distortions for plans and patients that that you know are not true.
We can’t afford politically skewed thought processes at this point in our history when we could be doing so much more and could actually cover everyone with better care for less money if we get this right.
Let’s set up an expectation of continuously improving care for our country and let’s use our Medicare cash flow to actually make it happen.